Non-Alcoholic Fatty Liver Disease
Home >Non-Alcoholic Fatty Liver Disease
Non-Alcoholic Fatty Liver Disease
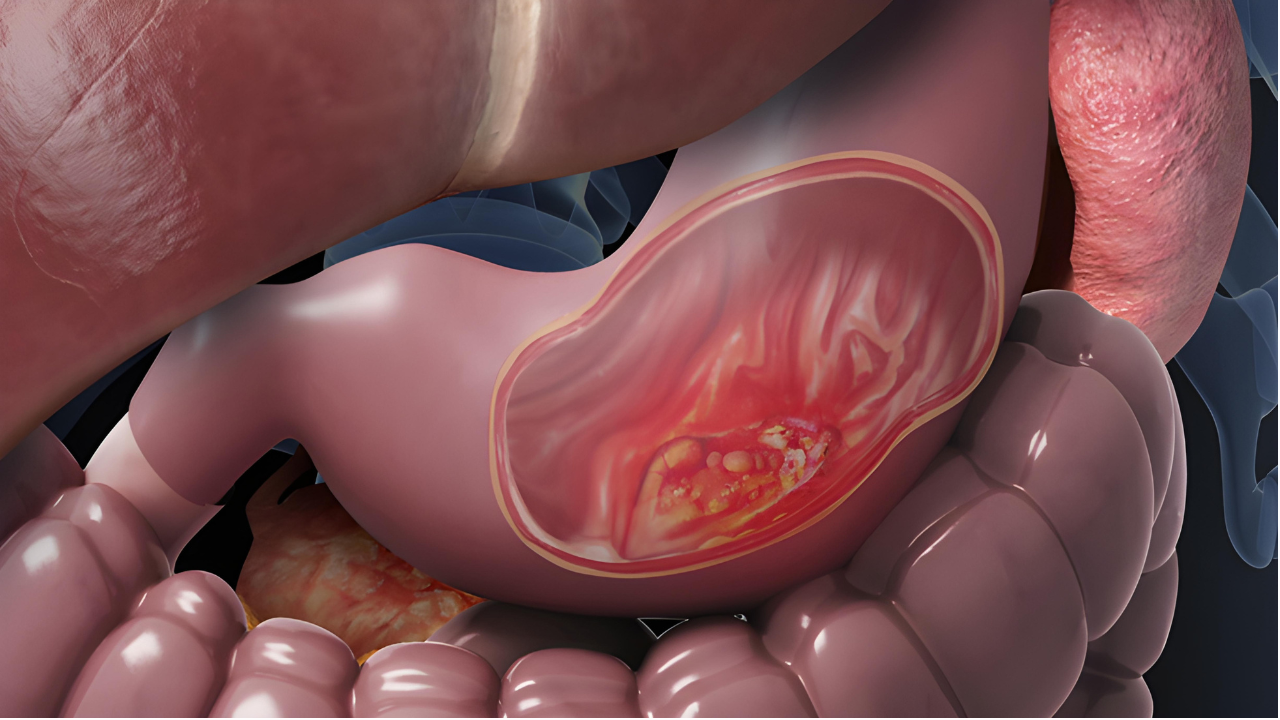
Non-Alcoholic Fatty Liver Disease (NAFLD) is a prevalent condition characterized by the accumulation of fat in the liver cells, not caused by excessive alcohol consumption. NAFLD encompasses a spectrum of liver disorders, ranging from simple fatty liver to more severe conditions like non-alcoholic steatohepatitis (NASH), which can lead to advanced liver complications.
Causes:
The development of NAFLD is multifactorial, with several contributing factors:
- Insulin Resistance: An impaired response to insulin leads to increased fat storage in the liver.
- Obesity: Excess body weight, particularly abdominal obesity, is a significant risk factor.
- Type 2 diabetes: elevated blood sugar levels and insulin resistance contribute to NAFLD.
- Metabolic Syndrome: Conditions like high blood pressure and abnormal cholesterol levels increase the risk.
- Genetic Factors: Some individuals may have a genetic predisposition to NAFLD.
- Dietary Habits: Diets high in refined carbohydrates and sugars, along with low fiber intake, can contribute.
Types of NAFLD:
1. Non-Alcoholic Fatty Liver (NAFL): involves fat accumulation without significant inflammation or liver cell damage.
2. Non-Alcoholic Steatohepatitis (NASH): characterized by fat accumulation, inflammation, and potential liver cell damage. NASH can progress to fibrosis or cirrhosis.
Symptoms:
In the early stages, NAFLD may be asymptomatic. As the disease progresses, symptoms may include fatigue, unexplained weight loss, abdominal discomfort, or elevated liver enzymes in blood tests.
Diagnosis:
- Blood Tests: Liver function tests measure enzyme levels indicative of liver health.
- Imaging Studies: Ultrasound, CT scans, or MRI visualize the liver and detect fat accumulation.
- Liver Biopsy: In some cases, a biopsy may be performed to assess liver damage and inflammation.
Treatment Approaches:
1. Lifestyle Modifications:
Weight Loss: Achieving and maintaining a healthy weight is paramount for managing NAFLD.
Dietary Changes: A balanced diet, low in refined carbohydrates and sugars, promotes liver health.
Regular Exercise: Physical activity improves insulin sensitivity and aids in weight management.
2. Medications: While no specific medications are universally approved for NAFLD, drugs targeting associated conditions (diabetes, high cholesterol) may be prescribed.
3. Management of Risk Factors: Controlling diabetes, hypertension, and dyslipidemia is crucial for NAFLD management.
4. Antioxidant Therapy: Some studies explore the use of antioxidants like vitamin E for managing NASH, but this should be done under medical supervision.
5. Bariatric Surgery: In cases of severe obesity and related NAFLD, weight-loss surgery may be considered.
Complications:
Untreated NAFLD can lead to complications such as NASH, cirrhosis, liver failure, and an increased risk of liver cancer.
Prognosis:
The prognosis for NAFLD varies, emphasizing the importance of early intervention. While NAFL may be benign, NASH poses a higher risk of complications. Lifestyle modifications, regular monitoring, and addressing associated conditions contribute to a better prognosis and improved liver health. Individuals diagnosed with NAFLD should work closely with healthcare professionals to develop a personalized treatment plan.
