Autoimmune pancreatitis
Home >Autoimmune pancreatitis
Autoimmune pancreatitis
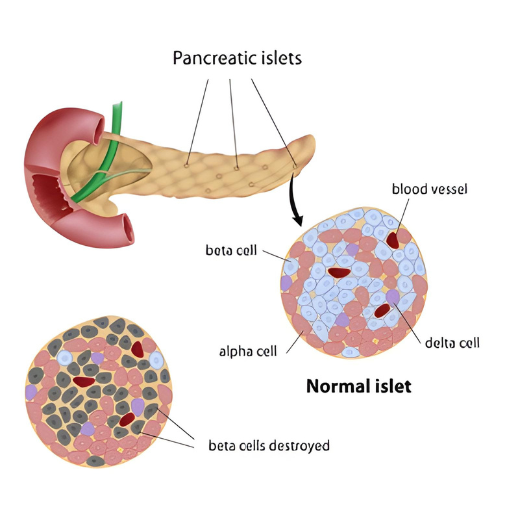
Autoimmune pancreatitis (AIP) is a rare type of chronic pancreatitis that occurs when the body’s immune system mistakenly attacks the pancreas. This condition leads to inflammation, scarring, and dysfunction of the pancreas. AIP is often characterized by abdominal pain, weight loss, and jaundice.
Causes and Risk Factors:
The exact cause of autoimmune pancreatitis is not well understood, but it is believed to be related to an abnormal immune response. Certain factors may contribute to the development of AIP, including genetic predisposition and environmental triggers. It is more common in men than women and is typically diagnosed in individuals over the age of 40.
Types of Autoimmune Pancreatitis:
Type 1 is more common and is often associated with elevated levels of immunoglobulin G4 (IgG4) in the blood. Type 2, on the other hand, is not typically associated with elevated IgG4 levels. Both types, however, respond well to treatment with corticosteroids.
Symptoms:
- Weight loss
- Nausea and vomiting
- Fatigue
- Changes in bowel habits
Diagnosis:
Diagnosing autoimmune pancreatitis can be challenging, as its symptoms can mimic other pancreatic disorders. Imaging studies such as CT scans and MRIs, along with blood tests to check for elevated IgG4 levels, are often used to aid in the diagnosis. A definitive diagnosis may require a biopsy of the pancreas.
Treatment:
1. Corticosteroids: The primary treatment for autoimmune pancreatitis is corticosteroids, such as prednisone. Patients typically respond well to corticosteroid therapy, and the dosage is gradually tapered over time.
2. Immunomodulators: In some cases, immunomodulatory medications, such as azathioprine or mycophenolate mofetil, may be used to help maintain remission and reduce the reliance on corticosteroids.
3. Biliary Stenting: If there is evidence of bile duct obstruction, a biliary stent may be placed to alleviate symptoms of jaundice.
4. Pain Management: Analgesics may be prescribed to manage pain associated with autoimmune pancreatitis.
Prognosis:
With appropriate treatment, the prognosis for autoimmune pancreatitis is generally favorable. Many patients experience significant improvement in symptoms and achieve long-term remission. However, a small percentage of individuals may experience relapses.
Conclusion:
Autoimmune pancreatitis is a rare and complex condition that requires a multidisciplinary approach involving gastroenterologists, immunologists, and other specialists. Early and accurate diagnosis, followed by prompt initiation of treatment, plays a crucial role in managing the disease and improving the quality of life for individuals affected by autoimmune pancreatitis.
