Acute Pancreatitis
Home > Acute Pancreatitis
Acute Pancreatitis
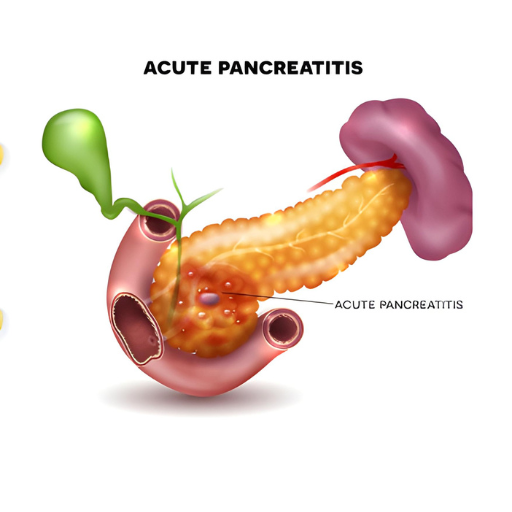
Acute pancreatitis is a sudden inflammation of the pancreas, a vital organ located behind the stomach. When the pancreas becomes inflamed, it can lead to severe complications.
Causes:
1. Gallstones: One of the most common causes of acute pancreatitis is the presence of gallstones, which can block the pancreatic duct.
2. Alcohol Consumption: Excessive alcohol intake is another major contributor to pancreatitis.
3. Trauma: Injuries or surgery to the abdomen may lead to inflammation of the pancreas.
4. Infections: Viral or bacterial infections can cause pancreatitis.
5. Genetic Factors: Some individuals may be predisposed to pancreatitis due to genetic factors.
6. High Triglyceride Levels: Elevated levels of blood triglycerides can also be a trigger.
Symptoms:
1. Severe Abdominal Pain: The hallmark symptom of acute pancreatitis is intense, sudden-onset abdominal pain, often radiating to the back.
2. Nausea and Vomiting: Patients may experience nausea and vomiting.
3. Fever and Rapid Heart Rate: Inflammation can lead to fever and an increased heart rate.
4. Abdominal Tenderness: The abdomen may be sensitive to touch.
5. Jaundice: In severe cases, jaundice (yellowing of the skin and eyes) may occur.
Diagnosis:
1. Medical History and Physical Examination: A healthcare provider will inquire about symptoms and perform a physical examination.
2. Blood Tests: Elevated levels of pancreatic enzymes in the blood, such as amylase and lipase, indicate pancreatitis.
3. Imaging Tests: CT scans or MRIs may be used to visualize the pancreas and detect inflammation.
4. Endoscopic Retrograde Cholangiopancreatography (ERCP): In certain cases, an ERCP may be performed to identify and treat gallstones or other blockages.
Treatment:
1. Hospitalization: Acute pancreatitis often requires hospitalization to manage symptoms and complications.
2. Fasting: Patients are usually kept from eating or drinking for a short period to allow the pancreas to rest Pand heal.
3. Pain Management: ain relief is crucial and may involve medications.
4.Addressing Underlying Causes: If gallstones or other factors are identified, they are treated to prevent recurrence.
5. Fluid Replacement: Intravenous fluids are administered to prevent dehydration.
6. Nutritional Support: Once the inflammation subsides, a gradual reintroduction of food is initiated, and nutritional support may be necessary.
In severe cases, complications like pancreatic necrosis or infection may require surgery. It’s essential to seek prompt medical attention for suspected acute pancreatitis to improve the chances of successful treatment and prevent complications. Additionally, lifestyle changes, such as reducing alcohol intake and maintaining a healthy diet, may be recommended to prevent recurrence.
