Alcoholic Liver Disease
Home >Alcoholic Liver Disease
Alcoholic Liver Disease
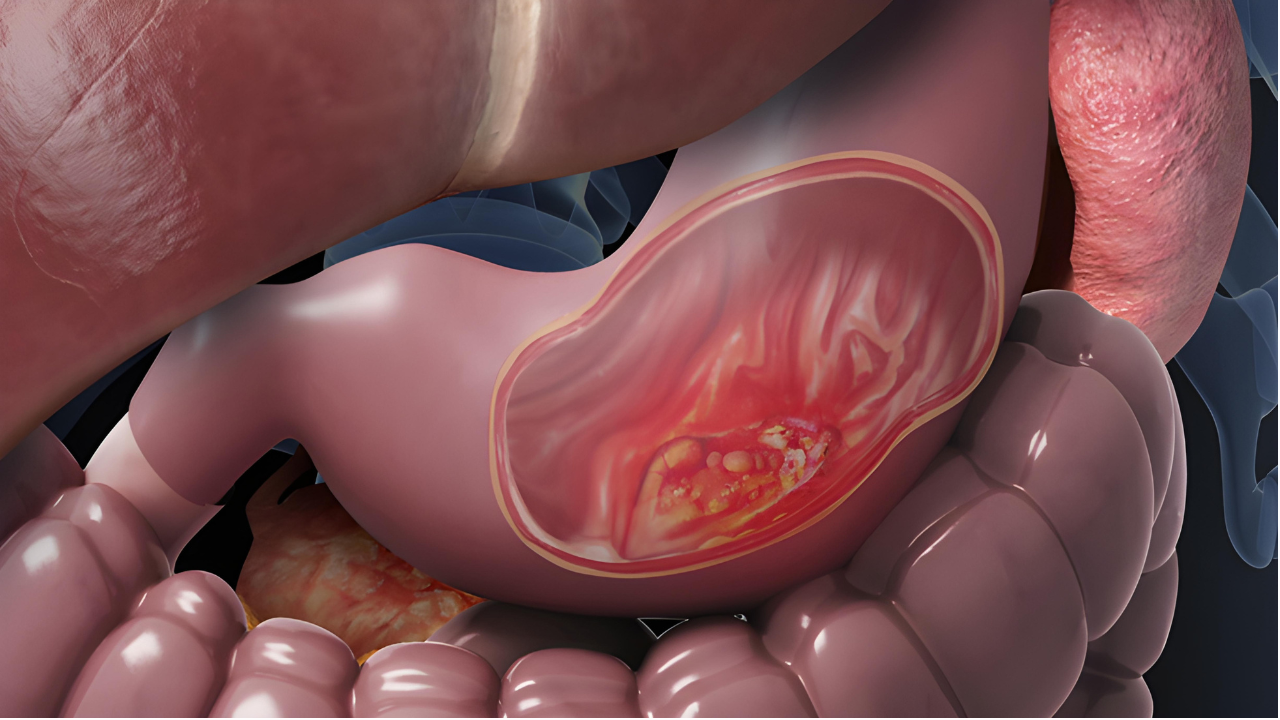
Alcoholic Liver Disease (ALD) is a spectrum of liver disorders caused by excessive and prolonged alcohol consumption. It encompasses various conditions, including fatty liver, alcoholic hepatitis, and cirrhosis, each representing a stage of liver damage. ALD is a leading cause of liver-related morbidity and mortality worldwide.
Causes:
The primary cause of ALD is chronic and heavy alcohol consumption. The liver processes alcohol, but excessive intake can overwhelm its ability to metabolize the substance efficiently, leading to inflammation, oxidative stress, and damage to liver cells.
Stages of Alcoholic Liver Disease:
- Fatty Liver (Alcoholic Steatosis): Accumulation of fat in liver cells is an early stage of ALD.
- Alcoholic Hepatitis:Inflammation of the liver tissue characterizes this stage, leading to symptoms such as jaundice, abdominal pain, and liver dysfunction.
- Cirrhosis: Prolonged liver damage results in the scarring of liver tissue, leading to cirrhosis. This advanced stage of ALD can lead to liver failure and has a higher risk of complications, including liver cancer.
Symptoms:
The symptoms of ALD can vary based on the stage but may include:
- Fatigue and weakness
- Jaundice (yellowing of the skin and eyes)
- Abdominal pain and swelling
- Nausea and vomiting
- Loss of appetite and weight loss
- Confusion and difficulty concentrating
Diagnosis:
Diagnosing ALD involves a combination of medical history, physical examination, blood tests to assess liver function, imaging studies (ultrasound, CT scans), and sometimes a liver biopsy to evaluate the extent of liver damage.
Treatment:
- Alcohol Cessation: The cornerstone of ALD treatment is complete abstinence from alcohol. This is crucial to prevent further liver damage and allow for potential recovery, especially in the early stages.
- Nutritional Support: Malnutrition is common in individuals with ALD. Nutritional support, including a well-balanced diet and sometimes vitamin supplements, is essential to address deficiencies and support liver function.
- Medications:
Corticosteroids: In cases of severe alcoholic hepatitis, corticosteroids may be prescribed to reduce inflammation. - Pentoxifylline: Another medication used in severe alcoholic hepatitis to decrease inflammation.
- Liver Transplantation: In cases of advanced cirrhosis where the liver is significantly damaged and not responsive to treatment, liver transplantation may be considered.
- Management of Complications: Treatment also involves managing complications such as ascites (fluid accumulation in the abdomen), encephalopathy (brain dysfunction), and portal hypertension, which can accompany advanced liver disease.
Prevention:
Preventing ALD primarily involves moderating or abstaining from alcohol consumption. Regular medical check-ups and screenings for liver function can help identify early signs of liver damage.
Prognosis:
The prognosis for ALD varies based on the stage at diagnosis, adherence to abstinence from alcohol, and the presence of complications. Early intervention and lifestyle changes can improve outcomes, but advanced stages may have a poorer prognosis.
In conclusion, Alcoholic Liver Disease is a serious and potentially life-threatening condition resulting from chronic alcohol abuse. Timely diagnosis, alcohol cessation, and appropriate medical management are essential for preventing further liver damage and improving outcomes for individuals affected by ALD.
